This is an example of an OSCE module that I thought would work well, but it didn’t.
The module suffered from over-reach, both in terms of the students’ capabilities, and also the application of simulation. Let me tell you about it.
I had been serving as one of the faculty at the M3 OSCE at a neighboring medical school, and one of the OB modules impressed me. A student entered the exam room and performed a routine OB visit on a live patient at 30 weeks. The visit was viewed remotely by faculty and graded by them.
Everything with the patient was normal, except for a size/date discrepancy of about 5 weeks. The student was then expected to counsel the patient about the significance of this and outline a plan for dealing with the problem.
My OSCE module was based on that experience, but changed to reflect the different resources available at my own institution.

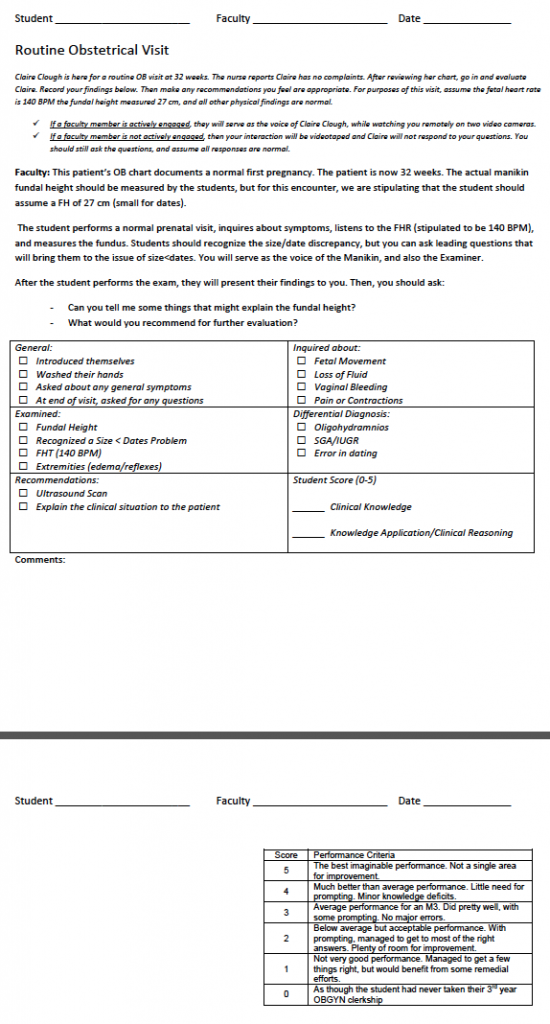
Instead of a live patient, I used a manikin, with remote faculty serving as the voice of the manikin. Students were provided this descriptor before entering the room. They had 15 minutes for the entire module.
Student-1-Routine OB visit at 32 weeks (pdf)
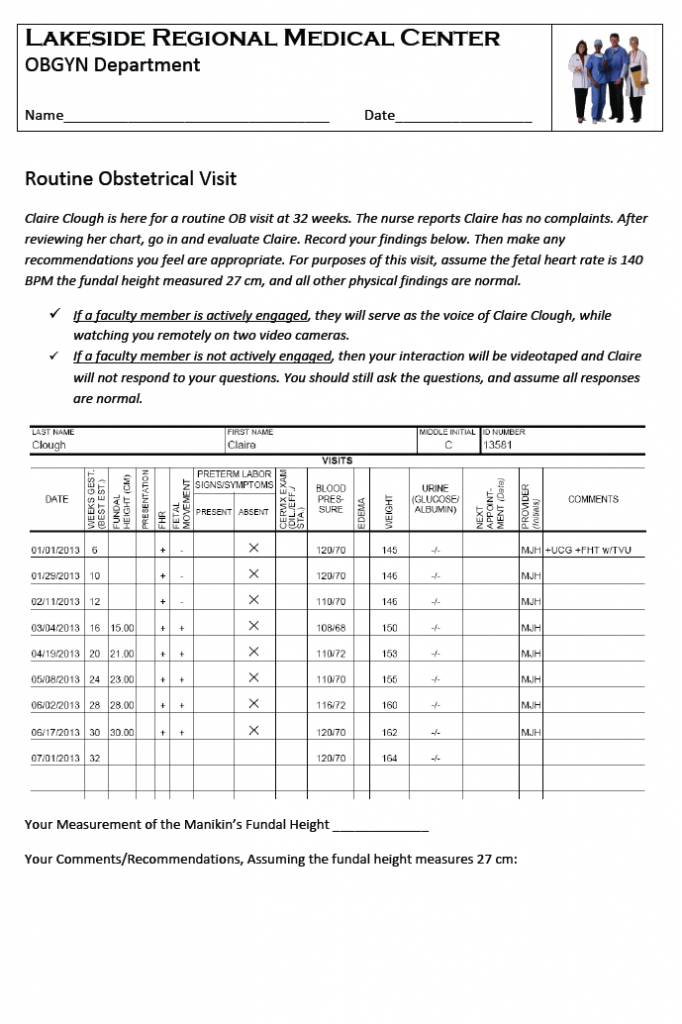
They were also provided a paper chart of the pregnancy records (all normal.)
Claire Clough Prenatal Records (pdf)
Rather than counseling the patient, the student was asked to write down their clinical findings, and plans for the patient.
The students were then graded on both their written responses, and their patient interaction, as viewed by the faculty remotely. We used these grading sheets:
Faculty-1-Routine OB visit at 32 weeks (pdf)
The feedback on this module from both students and faculty was uniform. There were a lot of problems.
- It took too long for the student to review the entire prenatal record, even though the findings were all normal.
- Because I was uncertain whether I’d have enough faculty to staff this module, I tried to have it both ways…with and without faculty. In the event, we had faculty, but I think that without faculty, it would not have worked at all.
- Because I gave instructions in the descriptor for both with and without faculty, the descriptor was confusing.
- Using the faculty remotely as the manikin voice was not a particularly good use of their skills. We decided it would be better to place the faculty in the room with the student and discuss the manikin findings. In this sense, the manikin would be used more as a prop, and less as an interactive tool.
- The obstetrical belly we used is a strap-on belly for clothing manikins. It looks OK from a distance, but it’s not a good fundal height measuring tool, because the boundaries (symphysis and fundus are unclear.
- The students were confused about the fundal heights. They were asked to measure the fundus, but then told to ignore that finding and instead assume a different measurement. They didn’t understand whether that meant their own measurement was incorrect or not.
- While all the students had a general understanding of the clinical problem of small-for-dates, none of them had any experience in documenting these clinical findings, or ordering appropriate followup. In the clinics, these tasks were assumed by the residents, who may or may not have used their experience for teaching the students.
Lessons Learned
- The best use of faculty is a one-on-one interaction, in person, with the student. Even though we have interactive manikins doesn’t mean we always should use the interactivity. It is OK to use them as props to promote discussion.
- While it is OK to have contingency plans in the event there are insufficient numbers of faculty to staff a module, those plans should be transparent to the students. With this module, I should have had two separate descriptors ready, but only used the one that I needed.
- It’s not a good idea to have the students review an entire prenatal record. They aren’t used to doing it quickly, and it burns up too much time during the module. If there is important information in the PN records that applies to the module, it’s better to include that information in the descriptor, in a brief, summarized fashion.
- Because our M3s get very little practice in actual order writing, it’s better to have them answer with general recommendations, rather than specific orders.